Posted July 2019 by Brandy V., B.S. Health Administration; M.A. English, Creative Writing; 9 updates since. Reading time: 8 min. Reading level: Grade 10+. Questions on monitoring brain function? Email Toni at: editor@online-psychology-degrees.org.
The brain is the most complex organ in our body. Its intricate systems consist of millions of different neurons with just as many channels of communicating. How these neurons communicate controls everything about us, from our movements to our mental health.
As a result, scientists have developed several tests that map and analyze our brains, each with their own purpose. Some tests measure how well the neurons in our brain are working, others measure the blood flow in our brain, and some measure multiple functions of the brain.
Scientists need these tools and much more to understand neurodegenerative diseases, neurological disorders, behavior disorders, cognition, and many other factors that affect the way our brain and body function.
Computed Axial Tomography (CAT) or Computed Tomography (CT)
Computed Axial Tomography (CAT), now often referred to as computed tomography (CT), is an advanced type of X-ray that takes detailed images of the body. Although it is most often used to analyze the skeletal structure for injury or abnormalities, it can be used to detect tumors, infections, some injuries, and diseases in the brain.
A CT scan is noninvasive, takes about 15 to 20 minutes, and transmits a 2D image onto a computer screen. It also provides more detailed information than a standard X-ray and is commonly used to analyze the brain from different angles which may aid physicians in understanding and treating abnormalities in the brain.
A CT scan is often used in conjunction with other tests, such as a standard X-ray or MRI for a multitude of reasons whether it’s to better understand an abnormality or to track the progress of a brain tumor. Doctors may use a CT alongside other tools to guide them during extensive surgeries too.
Magnetic Resonance Imaging (MRI)
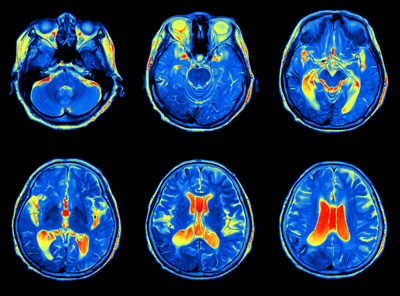
Magnetic resonance imaging (MRI) is one of the most common forms of evaluating soft tissue and organs. It utilizes a strong magnetic field and radio frequency to capture intricate images of the brain that are transferred to a computer screen.
More specifically, The National Institute of Biomedical Imaging and Bioengineering explains,
MRIs utilize power magnets that produce a strong magnetic field, forcing protons in the body to align with that field. When a radiofrequency current is pulsed through the patient, the protons are stimulated, and spin out of equilibrium, straining against the pull of the magnetic field. When the radiofrequency field is turned off, the MRI sensors can detect the energy released as the protons realign with the magnetic field.
An MRI is used for multiple reasons which include, detecting tumors, cysts, bleeding, infection, inflammation, injury, and swelling; determining the cause of headaches or migraines, dizziness, impaired vision, and seizures; and to choose effective treatments for abnormalities and injuries of the brain.
Functional Magnetic Resonance Imaging (fMRI)
Functional magnetic resonance imaging (fMRI), is another test people are familiar with in regards to brain mapping and monitoring brain anatomy. Like MRI, fMRI uses a magnetic field and radiofrequency pulses to record blood flow in the brain. The results are then translated onto a computer screen. Unlike an MRI, functional magnetic resonance imaging analyzes how blood flow in the brain changes with different activities.
The Center for Functional MRI explains the science behind an fMRI, “the nucleus of a hydrogen atom behaves like a small magnet. Using the phenomenon of nuclear magnetic resonance (NMR), the hydrogen nuclei can be manipulated to generate a signal that can be mapped and turned into an image.”
In simple terms, scientists know when your brain responds to stimulation whether it be reading, watching TV, speaking, or doing nothing at all, neural activity increases in the areas of the brain that control these functions. As a result, your brain increases blood flow and oxygen to these areas, and fMRI shows which parts of the brain are being used the most during a given stimulation. This, in turn, allows the evaluator to differentiate between gray matter, white matter, and cerebral spinal fluid.
Doctors and scientists use functional magnetic resonance imaging to evaluate the sections of the brain that are controlling essential functions and to analyze the extent of stroke, neurodegenerative diseases, injury, tumors, and disabilities. Doctors also use fMRI to determine the best therapy for a patient with brain issues or to plan risky surgeries involving the brain.
Electroencephalography (EEG)
An EEG measures neural activity generated by the numerous cortical layers of the brain. The test is either done by placing electrodes to the scalp or to an elastic cap depending on what portions of the brain need to be tested and how quickly those results need to be transferred to a graph or computer monitor.
According to Johns Hopkins Medicine, an EEG is used to detect problems with the brain, such as:
Seizure disorders like epilepsy, stroke, tumors or lesions (depending on the location and size of the lesion), Alzheimer’s disease, some psychoses, and narcolepsy. An EEG is also used to evaluate trauma, drug intoxication, the extent of brain damage, and used to monitor blood flow during brain surgeries.
In addition, an EEG may be used to measure a patient’s response to certain conditions or stimulations and confirm brain death.
The duration and process for an EEG depends on which type of EEG the patient needs. The most common EEGs are:
- A Routine or Standard EEG: This EEG last between 45 minutes and up to 3 hours depending on why the patient needs testing.
- An Ambulatory EEG: The patient wears a portable EEG recorder for 1 to 3 days, then documents their activities for the duration of the test. The evaluator compares the EEG’s recordings to each activity.
- EEG-Video monitoring: An EEG-Video is conducted at specialty medical clinics, takes several days, and is often used to diagnose critical neurological disorders.
Magnetoencephalography (MEG)
Magnetoencephalography (MEG) is similar to fMRI in that records the magnetic field generated by neural activity, but it is a much more sensitive form of neuroimaging. MEG has a fast and high temporal and spatial resolution, giving evaluators images of direct neural activity within milliseconds.
Furthermore, MEG is one of the most technologically advanced and recent forms of brain mapping that poses little risk to the patient. Its precision allows scientists to gain detailed information about sensory, motor, language, and memory cortex functions. According to MEGCommunity.Org, “MEG utilizes a superconducting quantum interference device (SQUID) technology, a sensitive detector of magnetic flux. ”
MEG is used to evaluate neurons that are functioning adequately and those that are malfunctioning which leads doctors and scientists to diagnose neurological issues like epilepsy. It is also used to analyze how the brain responds to different forms of stimulation.
What’s even more impressive is that MEG, MRI, and EEG can be used together to better understand the brain’s anatomy and function, leading doctors to more accurate diagnoses and treatment.
Electrocorticography (ECoG)
An electrocorticography (ECoG) is a procedure that monitors cognition, sensory and motor responses in the cerebral cortex through electrodes that are directly implanted on the brain’s surface. Even though ECoG is an invasive procedure it has its purpose in the medical field.
ECoG is commonly used to protect the brain as surgeons remove tumors or biopsy the brain. It also provides scientists with higher spatial and temporal resolution than some of the previously mentioned tests and scans.
According to the Journal of Neuroanaesthesiology & Critical Care, “ is commonly used for localization of epileptogenic focus during surgical treatment of epilepsy.” However, the Journal of Neuroanaesthesiology & Critical Care further explains that epilepsy surgery is only successful when the entire epileptogenic zone is removed.
ECoG can give doctors and scientists a more accurate image of the brain and how it’s functioning, but the risks of anaesthesiology and surgery make it a less than optimal procedure for evaluation and diagnosis.
Positron Emission Tomography (PET)
Positron Emission Tomography (PET) evaluates the brain’s blood flow, neurotransmitters, and chemical activity. It is often paired with CT or MRI scans to gain a full view of brain function. During a PET, the patient is given a mildly radioactive tracer (a dye when the brain is being monitored) which highlights activity in the brain.
PET enables scientists and physicians to monitor changes in the brain for a period of time, informing them about the progress of a disease or how a patient is responding to a stimulant. They may also use PET to determine if a growth in the brain is benign or malignant. Through positron emission tomography, scientists are able to understand some of the most debilitating brain issues such as stroke, dementia, Alzheimer’s, and Parkinson’s
Science has come a long way since we first began monitoring the brain and even though we still have much to learn, these tools allow scientists to understand brain function and anatomy. More importantly, these tools allow doctors to more accurately diagnose and treat brain abnormalities, diseases, and disorders.
More Related Articles:
- Important Terms To Know In The Psychology Classroom
- What Does Evolution Teach Us About Psychology?
- 5 Learning Theories in Psychology
- 5 Key Facts About Psychology in the 21st Century